Contraception: Your perceptions of the pill
In a world where personal choices and reproductive health go hand in hand, contraception stands as a vital pillar of informed decision-making. The choices we make regarding contraception not only influence our individual lives but have far-reaching implications for our partners and society as a whole.
In a study of over 2000 sexually active UK adults, our team of experts wanted to investigate the British public's views of contraception, aiming to provide a better understanding of this critical aspect of sexual and reproductive health.
What methods of contraception do people use?

To understand the most popular contraception methods in the UK, we first investigated public attitudes towards preventing unwanted pregnancies.
The most common forms of contraception were condoms and the contraceptive pill, with 58% and 47% of respondents reporting they have used these methods since becoming sexually active.
Surprisingly, our survey found that more than one in seven sexually active UK adults (14.4%) have never used any form of contraception. During sexual encounters, 17% of men choose not to use contraceptives with their partners, while 12% of women make the same decision. The statistics highlight the complexity of personal decision-making, influenced by factors such as access, availability, knowledge, beliefs, and education.
Among the younger population, especially those between the ages of 18 and 24, over a quarter (27%) have also resorted to emergency contraception. This age group used the morning-after pill more frequently than any other generation, with 22% of 25 to 34-year-olds coming in a close second.
Regarding intrauterine devices (IUDs), this seems to be slightly less popular with younger generations and more prevalent among Millennials and Gen X (12% and 12.5% respectively). Finally, our study found that approximately 1 in 10 women have used hormonal implants since becoming sexually active.
These findings underscore the importance of comprehensive discussions on contraception and its far-reaching implications. Talking about contraception can increase awareness of contraception's impact on reproductive health, relationships, and societal factors. Acknowledging the implications of each method can lead to informed choice, sexual health, gender equality, and family planning. Whenever you’re considering new methods of contraception, it’s vital that you consult with your doctor as every person's body is different - some products are more effective than others and each has different side effects.
What methods have worked well in the past?
In the following section, we will explore the various contraceptive methods deemed effective and reliable by survey respondents. This examination will provide valuable insights into the complex landscape of contraceptive practices.
Alarmingly, 29% of those aged between 18 to 24 believed that the pull-out method is an effective method of preventing pregnancy. Dr Babak Ashrafi, a GP at ZAVA UK, explains that this could be due to a range of factors:
“Younger generations may perceive the pull-out method (also referred to as the withdraw method) as an effective form of contraception for several reasons, such as a lack of comprehensive sexual education, social and peer influences, a misunderstanding of pre-ejaculation, a desire to avoid hormonal methods or a lack of awareness of failure rates.”
“The pull-out method, while better than no method at all, is considered one of the least effective forms of contraception. In reality, it does not provide adequate protection against unwanted pregnancies or contracting a sexually transmitted infection (STI). To address these misconceptions, comprehensive and accurate sex education, open communication, and access to a range of contraceptive options are essential for younger generations to make informed choices about their sexual health.”
According to the survey, the majority of respondents (83%) believed that condoms are the most effective way to prevent unwanted pregnancies. The contraceptive pill was believed to be the second most effective method, with 81% of respondents considering it reliable. Sterilisation methods, including vasectomy for men and tubal ligation for women, were considered efficient by 78% of the participants.
As we’ve learnt above, it is essential to provide comprehensive sex education to young people before they start having sex and begin using contraception. In the following section, we will examine the primary methods used by the British to learn about sex education.
How the UK gathers information about sex education

Before discussing the effectiveness of sexual education in Britain, it's crucial to identify peoples’ primary sources of information. Our study reveals that 22% of the UK say the internet is their primary resource for contraceptive information, with over a third of 18-24-year-olds stating that they learn about contraception online - via the use of search engines or through social media.
Less than half (40%) of British adults consult a medical professional about contraception, with this figure dropping to less than a third for men (31%). Three-quarters of male respondents also said they were either not taught or unsure whether they were taught about talking to a partner about sex in school. An even larger percentage of male participants were also not taught about erectile dysfunction in school (83%), and 80% of men were never taught about premature ejaculation.
Women were much more inclined to talk to a medical professional about contraception, with over half of female participants (53%) stating that they gained their knowledge of sexual health by speaking to a doctor, nurse or sexual health advisor about contraception. Over 1 in 10 women also said that they talk to their friends and family about contraception.
The role of sex education
The way sexual education is delivered in the UK can have a far-reaching impact that may not be immediately apparent. Inadequate education among younger generations can result in various personal sexual health issues, including an increase in STIs, unintended pregnancies, and sexual violence. Additionally, it can give rise to more extensive societal challenges, such as higher healthcare expenses, added pressure on childcare services, and greater gender inequality.
To understand how sexual education is taught across the UK, we asked whether respondents had been taught about contraception whilst at school. We also expanded our questions to consider whether consent has been taught consistently across generations.
How contraception is taught in schools across the UK
According to our survey, the prevalence of contraceptive education in schools varies widely across the country. Respondents from Norwich answered that they did receive information on contraception in school, with over 74% saying they were taught about it during sex education. Next on the list were respondents from Bristol (69.2%), with Newcastle (67.3%), Birmingham (66.8%), and Nottingham (65.1%) rounding off the top 5 cities that stated their sex education included contraception.
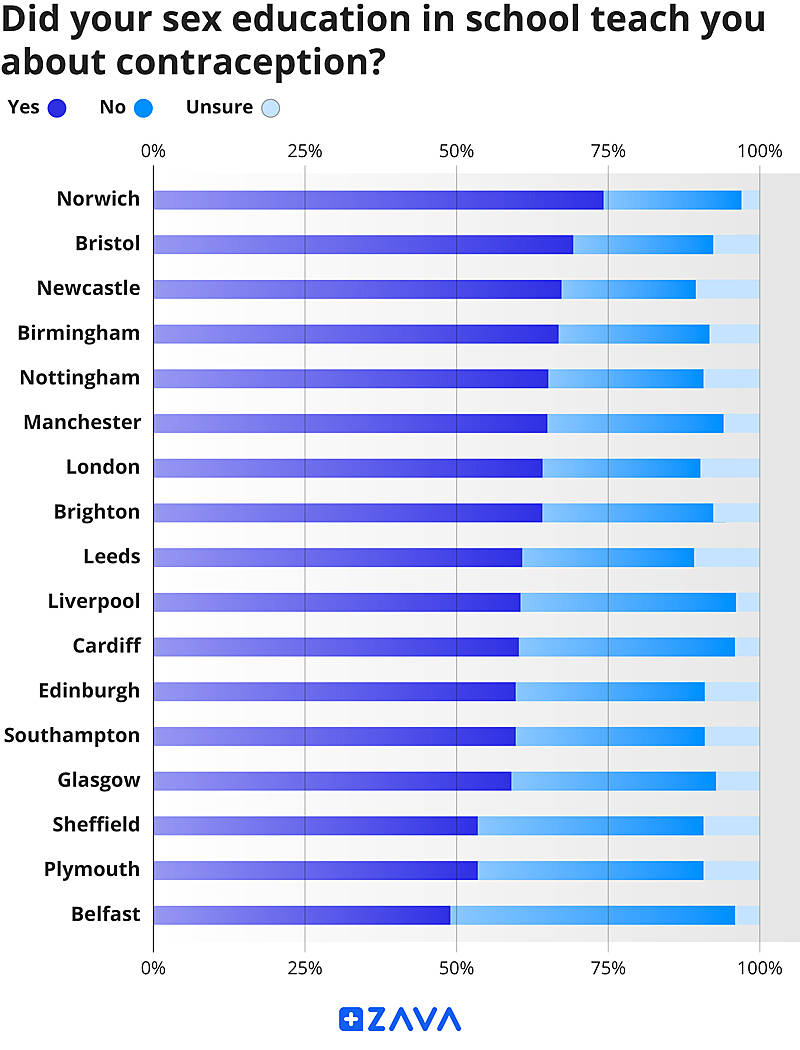
Belfast stands as the only city in the UK where less than half of respondents weren’t taught about contraception during sex education, with 46% stating that they did not receive any contraceptive information at school. Plymouth and Sheffield came just above the halfway mark at 53% and 56%, with Glasgow sitting at the bottom of Scottish cities.
Addressing consent
When discussing sexual education, we wanted to understand all aspects that might have been taught at school. One area we asked about was sexual consent. Our research uncovered that the concept of consent has become a much wider-taught subject in recent years but much less common among older generations.
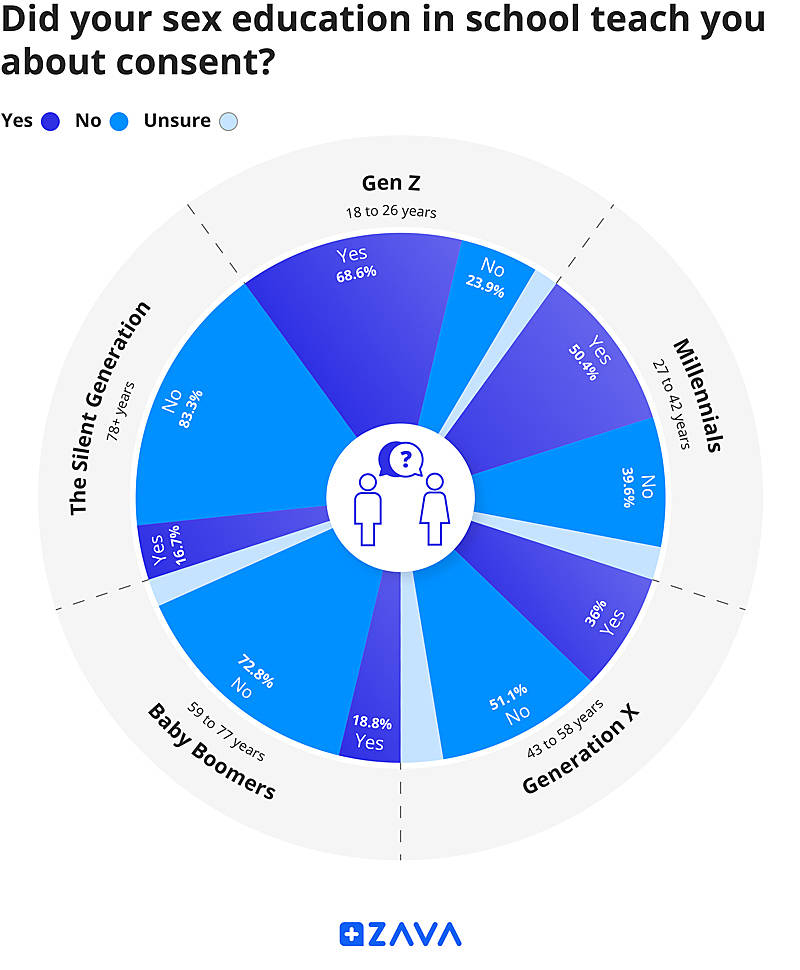
Gen Z leads the way when it comes to learning about sexual consent. Over two-thirds of respondents stated that they received education about consent in school, compared to less than a quarter who said they did not. The majority of Millennials indicated that they received education on consent in school, with 50% affirming and 40% negating this. Changing societal norms, increased awareness of consent issues, and the #MeToo movement have contributed to greater education about consent among younger generations.
When analysing respondents over the age of 42, a different picture emerges. 51% of Gen X, 72% of Baby Boomers, and 83% of the Silent Generation responded that they did not receive education about consent in school. These statistics do not suggest that older generations have never asked for consent before engaging in sexual activities. However, they do indicate a historical lack of awareness and understanding of the significance of sexual consent.
How much do people know about contraception?
Contraception has the potential to empower individuals and enhance their quality of life in many ways. It allows couples to plan and space their pregnancies and enables women to pursue their educational and career goals without the constraints of unplanned pregnancies.Hormonal contraception can also help regulate menstrual cycles, alleviate menstrual pain and reduce the risk of certain health conditions such as ovarian cysts, endometrial cancer, and anaemia.
After exploring the vast array of resources available for sexual education, we sought to gain insight into people's knowledge of contraception. Our goal was to gain a better understanding of how we can improve sexual education. To do this, we presented our survey participants with a range of statements and asked them to tell us whether they believed them to be true or not.
In fact, all of the below statements are actually false:
“Condoms are only effective for preventing pregnancy.”
In our survey, this statement was agreed with by nearly 1 in 5 participants. This shows respondents were unaware that condoms are also effective for the use of preventing STIs. This barrier of protection made of latex or polyurethane material prevents STIs, such as HIV, chlamydia and gonorrhoea, from passing from one sexual partner to another. It is, however, only effective when applied consistently and correctly, ensuring there are no tears or holes in the condom, and using adequate lubrication to avoid breakages.
“All contraceptive methods require a prescription from a healthcare provider.”
15% of Britons believed this statement was true, with this rising to over a fifth of Gen Z and 17% of Millennials. Condoms are a prime example of a contraceptive method that does not require a prescription, although it’s wise to discuss with a doctor whether you’re allergic to materials such as latex before use. Additionally, an implant can be administered at a sexual health clinic without a prescription. Many methods do require a prescription in the UK, such as combined oral contraceptives or progestogen-only pills. As always, you should always consult your doctor before trying any new method of contraception.
“Contraceptive methods always have the same side effects for everyone.”
Over 1 in 5 people aged between 18-24 were under the impression that all contraceptive products had the same side effects on different people. In fact, contraceptives can have different effects on different people, so it is important to discuss potential side effects of contraception with a medical professional before use.
If you want to learn more, Dr Kathryn Basford explains various side effects of the contraceptive pill, such as nausea, breast tenderness, headaches, weight fluctuations, mood swings, and irregular bleeding in this article.
Who is responsible for contraception?
It is important to consider the beliefs and responsibilities of the British public in managing their reproductive health, especially when it comes to contraception. It directly affects individuals' well-being, as informed decisions on family planning impact their quality of life. Contraceptive choices have broad significance, influencing societal and healthcare systems and promoting gender equality, sexual autonomy, and informed consent.
In this section, we will examine the various perceptions surrounding responsibility for contraception. We will delve into societal norms, gender roles, and changing perspectives. We will shed light on the eagerly anticipated but elusive male contraception pill, which could be a game-changer in birth control, and discuss how it may impact the distribution of responsibility.
Our results found that the vast majority of Britons did not believe that women are more responsible for contraception than men (70%). When asked if men should take more responsibility for contraception, two-thirds of women agreed - this compared to just under half of men. The majority (75%) of survey respondents agreed that birth control should be a shared responsibility between sexual partners.
Currently, for men, there are only a handful of safe methods of contraception they can access - condoms, contraceptive gels or creams, or sterilisation. Male contraceptive methods are still in development and not yet widely available, but there is ongoing research and clinical trials for male hormonal and non-hormonal options, like the male contraceptive pill.
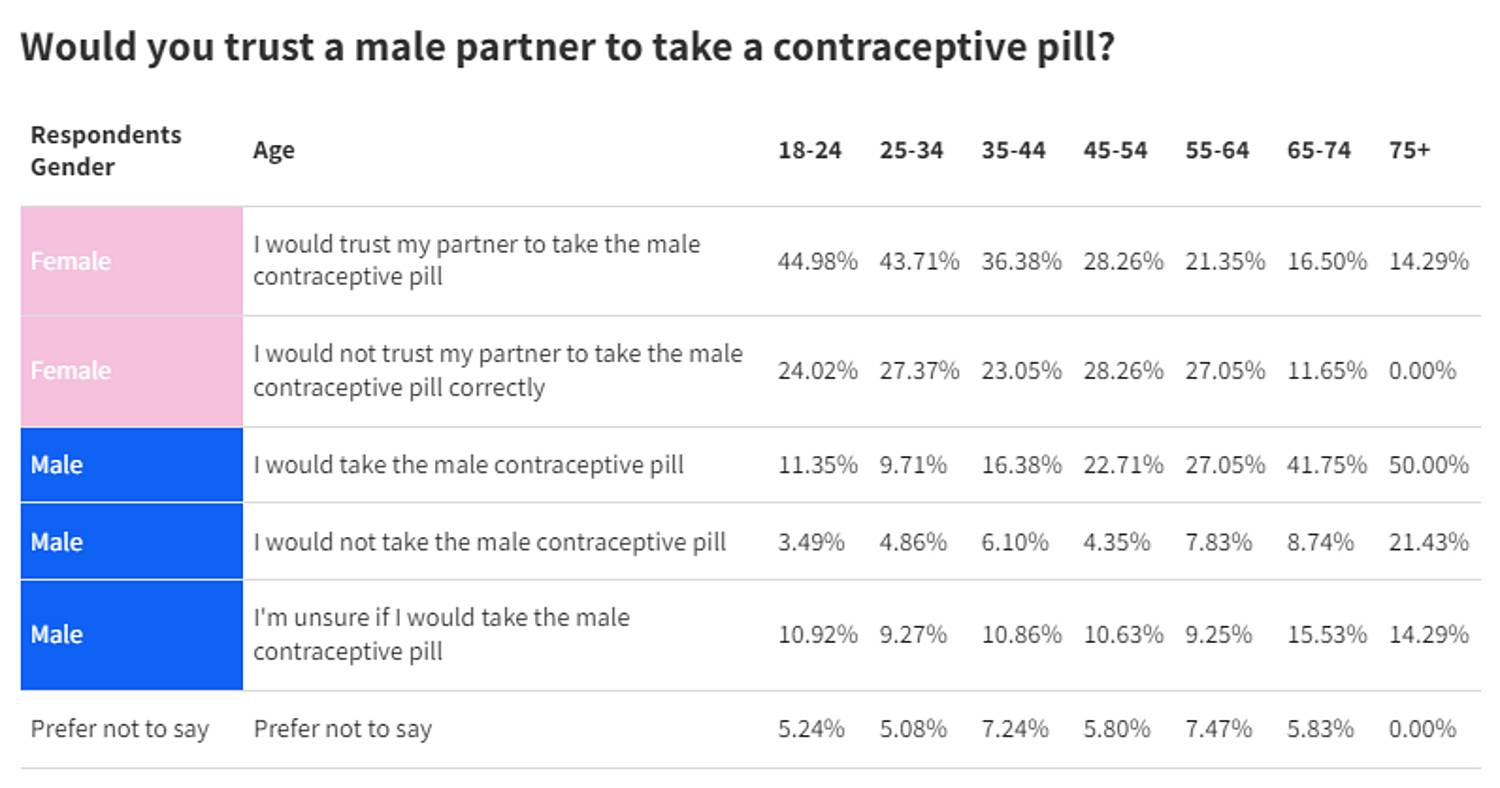
When asked about using a potential male contraceptive pill, results varied amongst the population. Female respondents were divided on whether they would trust a male partner to take a contraceptive pill, with 54% responding positively and 40% negatively. Less than half (45%) of men said they would take a male contraceptive pill if it became available, with a quarter saying they were unsure and 13% saying they would not take the pill. When split by age, the younger a respondent was the more trusting they were of their male partner to take a male contraceptive pill.
Final thoughts
Contraception is an important aspect of making informed decisions, with far-reaching implications for individuals and society. Our findings underscore the wide range of contraceptive methods available, but also the concerning number of sexually active adults who do not use any form of contraception.
Misconceptions about the effectiveness of certain methods still persist, especially among younger generations. Comprehensive sex education and open communication are essential to address these gaps. Our research highlights the importance of accessible and accurate sexual education. While the internet provides a major role in accessing information, especially for those who are new to sex, medical consultations, particularly among men, are less frequent. This reveals a need for better sex education resources.
In summary, this study reinforces the importance of informed decision-making, reducing misconceptions, and promoting open dialogues about contraception. Providing individuals with knowledge and access to various contraceptive options is crucial for well-being, relationships, and societal health. This will help us move towards a more informed, empowered, and equitable society.
Whether it’s your first time using contraception or you need to fulfil an existing prescription, our online doctor service gives you access to NHS-trained doctors without leaving the comfort of your home. Check out our full range of services and resources here.