Genital Warts Treatment
Get genital warts treatment from our doctors with free and fast delivery.
Prices from £34.99
Simply fill in a brief consultation questionnaire and one of our doctors will review your request today.
Genital warts are a sexually transmitted infection. Treatment for genital warts can involve a range of methods. ZAVA can provide a prescription for topical creams, suitable for small warts.
If you think you may have been infected you can complete our brief online questionnaire and choose your preferred treatment. Our doctor will review your request and approve appropriate treatment.
Prescription and delivery are included.


Genital Warts Treatment
Warticon
Active ingredient: podophyllotoxin.
Side effects: Your skin might feel mildly irritated when you apply it. You may also experience inflammation, ulcers, soreness, itching, redness or pain where the warts were. Skin problems may occur if Podophyllotoxin is left in contact with healthy skin.
Condyline
Active ingredient: podophyllotoxin.
Side effects: The same side effects as Warticon, as they both contain the same active ingredients.
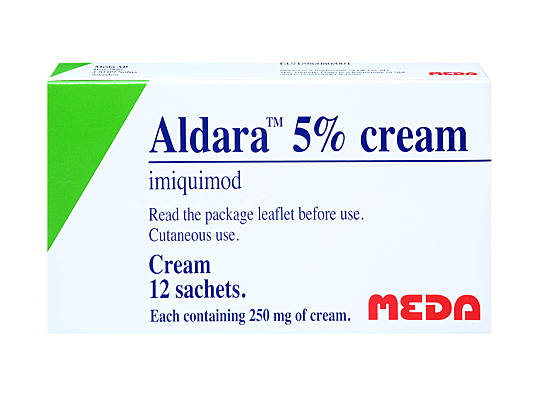
Aldara
Active ingredient: imiquimod.
Side effects: Can cause skin reactions and may damage healthy skin. Imiquimod does have some common side effects, which include: hardening of the skin and flakiness, swelling, a burning or itching sensation after applying the cream, and/or a headache. Normally these side effects are quite mild and they go away within two weeks of finishing treatment.
-
-
Genital Warts are caused by a viral skin infection called the human papillomavirus (HPV). They’re skin coloured bumps, fleshy growths or changes to the skin that appear on the genital area: on the penis, vagina or around the anus. They don’t normally hurt or cause any long term harm, but they can look unsightly and many people feel distressed by them. Genital warts are very common in England, and are the second most common sexually transmitted infection after Chlamydia.
The most common way for people to become infected is sex (vaginal or anal), but HPV can also be passed on via oral sex, sharing sex toys and non-penetrative genital to genital contact. A mother can also pass HPV to her baby when she gives birth.
-
-
Which treatment is best for you depends on the size and types of warts you have as well as which body parts are affected. Treatments range from topical creams that either boost your immune system or dissolve the wart, to surgical treatments (cryosurgery, surgical removal, electro-cauterization or laser therapy), or using a chemical acid that burns off warts. People react differently to different genital warts treatments. Some people will require several weeks of treatment, or several visits to the doctor to get rid of their warts.
If you are pregnant, make sure to tell your doctor or health care provider, since certain types of medications for genital warts may be harmful to the developing baby.
-
-
Do not use over-the-counter treatments for genital warts. These medications are for other types of warts (e.g. on the face or hands) and they'll only cause you pain and irritation. Unfortunately, genital warts are harder to get rid of and most often you will need a prescription medicine, from your dermatologist or your GP (online or otherwise). Your doctor will assess which treatment is best for you, depending on the number of your warts, their location and the state of your immune system.
-
-
The Health Protection Agency reports that, in 2017, there were 59,119 new cases of genital warts diagnosed at sexual health services in England. In the same year, there were 203,116 new cases of chlamydia.
Sexually active teenagers and young adults are the people who most commonly catch genital warts.
-
-
Genital Warts are caused by a viral skin infection called the human papillomavirus (HPV). HPV is a family of more than 100 viruses. The majority of people who have been infected with HPV do not know they have it, because they don’t have any symptoms. 9 out of 10 cases of genital warts are caused by just two strains of HPV (type 6 and type 11).
Other strains of HPV cause cervical cancer. The HPV vaccination, which is now offered to all girls at school when they’re 12 or 13 years old, protects against the strains of HPV that cause genital warts as well as against HPV types 16 and 18 (which cause over 7 out of 10 cervical cancers in the UK). It’s expected that from the beginning of the 2019-2020 school year this vaccine will also be offered on the NHS to boys 12 to 13 years old.
Genital warts are spread by skin to skin contact. You can catch them by having sex (anal or vaginal), but you can also catch them if you don’t have penetrative sex, but do have genital contact, oral sex, or if you share sex toys. A mother can also pass HPV to her baby when she gives birth.
It can take months or even years for the warts to appear if you’ve contracted HPV, so if your partner grows warts it does not necessarily mean they’ve been having sex with someone else recently.
You are more likely to pass the warts to someone else if you have skin to skin contact whilst the warts are there, but you can infect another person with the human papillomavirus before the warts appear or after they’ve gone. Using condoms can help to cover up some warts, but this won’t necessarily offer you full protection because the skin around your genitals can also become infected and won’t be covered by the condom.
-
-
Sexually active young adults are the people who most commonly catch genital warts: the highest rates are in men and women aged 20 to 24. The HPV vaccine has been having an effect though, since 2009 the rates of genital warts in women aged 15 to 19 has dropped.
-
-
Genital warts are diagnosed by a doctor or nurse looking at the area that you’re worried about. Usually no specific test is used or needed, the doctor or nurse can tell that it’s a wart just by looking at it. If it doesn’t look like a wart you might need to have some more tests.
In women, the warts can affect the cervix and inside the vagina, so usually a doctor will use something called a speculum to have a look inside and check for warts.
You can get a diagnosis at your local sexual health clinic, from your GP, or by using ZAVA’s photo assessment service.
-
-
Genital warts won’t usually cause you any harm in the long term. You might not like the way they look, they can be uncomfortable and their presence might be psychologically distressing. If you don’t treat your genital warts, in time they might go away by themselves. They might also grow, stay the same or multiply. Normally most warts disappear by themselves, in time, without treatment, but this can take a long time.
It is better to get the warts diagnosed and checked by a doctor, even if you don’t intend to treat them. If you are not trained, it is very easy to confuse a more serious growth for a wart, so you need to get a professional opinion to be sure.
-
-
It can take several months to get rid of genital warts, so you need to persevere with the course of treatment as advised.
Sometimes the area where the treatment has been used can become irritated or sore. After you complete the course of treatment, most side effects should have passed within 2 weeks.
-
-
Yes. Unlike treatments for other warts, you can’t buy treatment for genital warts over the counter. It is only available on prescription.
-
-
Yes. You can get treatment at your local sexual health clinic or from your GP. These clinics are available for everyone to use confidentially, regardless of age. They’re free.
-
-
Yes. If you are diagnosed with genital warts then it is better for your partner to go and get a check up, in case they also have warts that they might not have noticed.
-
-
You should avoid having sex whilst you’ve got genital warts. Instead, you should follow the treatment as prescribed and wait for it to take effect. You need to give the warts time to heal. Sex can make them bleed and slow down your recovery. By not having sex, you’ll recover more quickly. You’ll also be less likely to pass the warts on to your sexual partner.
Even after the warts have cleared up, you can still have traces of HPV in your skin cells. For this reason, to be on the safe side, use a condom for the first three months after the warts have cleared up.
-
-
There is no evidence to suggest that having genital warts will affect your fertility.
-
-
They're skin coloured bumps, fleshy growths or changes to the skin that appear on the genital area: on the penis, vagina or around the anus.
In women, genital warts normally start as small gritty lumps that grow larger.
In men, genital warts normally look more like the type of warts you might see on a person’s hand – raised, hard and with a rough surface.
People can have just one wart, or they might get a cluster of warts that together make up a sort of cauliflower formation.
-
-
A topical treatment is a cream, lotion, or a chemical that’s applied directly onto the wart or warts. This kind of treatment tends to work better on softer warts.
The most common topical treatments include:
- Podophyllotoxin (sometimes known as Condyline or Warticon): This works by poisoning the cells of the warts. It is recommended for small clusters of warts. It comes as a liquid and is dripped onto the wart using a special application stick. The skin might feel mildly irritated when you apply it. You have to put it on in cycles – so you apply it twice a day for three days, then take a rest cycle where you don’t apply the liquid for four days. Following this cycle, most people find it takes 4 or 5 weeks for their warts to clear up. It is generally very effective at clearing genital warts.
- Imiquimod (Aldara): This works by stimulating your immune system to fight off the warts. It is recommended to treat larger warts. It is a cream that you put onto the wart/warts. You wash it off 6-10 hours after you have applied it. You have to do that three times a week, for several weeks before you’ll see an improvement. Imiquimod does have some common side effects, which include: hardening of the skin and flakiness, swelling, a burning or itching sensation after applying the cream, and headaches. Normally these side effects are quite mild and they go away within two weeks of finishing treatment. Imiquimod is effective for about 50% of patients.
Note: The wart creams that you can buy over the counter in pharmacies are designed to deal with warts on your hands or verrucas on your feet. They’re not suitable for treating genital warts.
-
-
If topical treatments are not suitable or have not worked, there are other types of treatment available. Usually these will need to be carried out at a sexual health clinic.
In some cases, the nurse or doctor might suggest a combination of treatments. It can take several months to get rid of the warts, so you need to persevere and follow the course of treatment advised.
Cryotherapy – freezing warts off
Cryotherapy or freezing off the warts is usually suggested for treating groups of small warts, especially if they’re on/near the vulva or on the shaft of the penis.
Cryotherapy uses liquid nitrogen to freeze the wart. This kills the cells of the wart by splitting their outer membranes. After the wart is frozen, it is left to thaw out and, if necessary, the treatment is repeated. Whilst the warts are being frozen, you’ll feel a burning sensation. After the warts have been frozen, you’ll probably get some blisters, skin irritation and pain on and around the site of the wart.
It takes 1-3 weeks for your skin to heal after the wart has been frozen – don’t have sex until the skin has healed properly.
Excision – cutting warts away
Excision is where the warts are cut away. It’s normally used for small, hard warts or clusters of warts that have formed a cauliflower shape.
Before the procedure begins, you’ll be given a local anaesthetic. The wart will then be removed with a scalpel and the wound will be stitched up.
Excision can leave a scar, so it might not be the best option for large warts. The skin will be sore for 1-3 weeks afterwards. Avoid sex until the skin has healed fully.
Electrosurgery
Electrosurgery is normally used after excision if there’s a particularly large wart near to the anus or vulva, and if topical treatments haven’t worked.
In electrosurgery, most of the wart is cut away, then an electric current is passed through a metal loop which is pressed against the wart to burn away the remaining part of it.
If you’re having lots of warts removed in this way, it can hurt quite a lot, so often your doctor will give you a regional anaesthetic (that numbs you everywhere from below the spine down). In extreme cases, a general anaesthetic might be given.
Laser surgery
Laser surgery uses a laser to burn away warts that can’t be reached by other types of physical treatment – for example, if the warts are deep inside your anus or urethra. It’s done under local or general anaesthetic.
Laser surgery might also be suggested for pregnant women who did not have success with the topical treatment TCA.
You’ll probably be sore and find the skin is irritated at the site where you had the warts, but this should heal in 2 to 4 weeks.
-
-
It’s not understood why, but smokers tend to find the topical creams less effective at curing their genital warts than non-smokers. You might want to quit smoking to make your treatment more effective and to speed up your recovery.
Podophyllotoxin (sometimes known as Condyline or Warticon)
The skin might feel mildly irritated when you apply it. You may also experience inflammation, ulcers, soreness, itching, redness or pain where the warts were. Skin problems may occur if Podophyllotoxin is left in contact with healthy skin. Don’t use Podophyllotoxin anywhere other than the area of skin that is affected and needs treatment.
Talk to your prescriber before taking podophyllotoxin if:
- you’re allergic to any of the ingredients in the medicine,
- you’re breastfeeding or pregnant
- you’re currently using other preparations that contain Podophyllotoxin
- you have open wounds in the area where Podophyllotoxin needs to be applied
- the medicine is for a child
Imiquimod (sometimes known as Aldara)
Imiquimod can cause skin reactions and may even damage healthy skin. Speak to your doctor and read the Patient Information Leaflet.
Imiquimod does have some common side effects, which include:
- hardening of the skin
- flakiness
- swelling
- a burning or itching sensation after applying the cream
- headache
Normally these side effects are quite mild and they go away within two weeks of finishing treatment.
Some good steps to take while you’re using imiquimod include:
- protecting the treated areas of the skin from sunlight while you’re using it, as imiquimod can cause sensitivity
- not using Imiquimod for more than 16 weeks
- avoid contact with eyes, lips and nostrils
Talk to your prescriber before taking imiquimod if you:
- are allergic to any of the ingredients in the medicine
- are immunosuppressed
- have an autoimmune problem
- have blood problems
- have had an organ transplant
- have had treatment for this problem before
- have HIV infection
- have sore or damaged skin in the area where you are planning to apply Imiquimod
- have warts in the urethra, vagina, rectum, anus, cervix or under the foreskin
Imiquimod is usually not suitable for children and adolescents.

Dr Kathryn Basford is a qualified GP who works as a GP in London, as well as with ZAVA. She graduated from the University of Manchester and completed her GP training through Whipps Cross Hospital in London.
Meet our doctorsLast reviewed: 10 May 2019
-
Genital warts, National Health Service [accessed February 2023]
-
Aldara 5% Cream, Patient Information Leaflet, EMC [accessed February 2023]
-
Imiquimod, NICE/British National Formulary [accessed February 2023]
-
How effective is Aldara for genital warts? Drugs.com [accessed February 2023]
-
Information on HPV vaccination, GOV.UK [accessed February 2023]