STI symptoms in men

Medically reviewed by
Dr Babak AshrafiLast reviewed: 07 Jan 2022
Sexually transmitted infections (STIs) are infections that are passed on to you if you have any kind of sexual activity with an infected person. An STI can be caused by bacteria, viruses or a parasite. STIs are also known as sexually transmitted diseases (STDs) if you need long term treatment for them.
You might not always get symptoms if you have an STI, which can make it harder to remember to get tested. It's better to practice safe sex and get tested if you've ever had unprotected sexual contact.
Some STI tests require either one or more of a:
- swab, like for herpes
- urine sample, like for chlamydia
- blood tests, like for HIV or hepatitis B
Treatment for STIs can be as simple as taking antibiotics or antiviral medicines. While most treatment is only needed once, you may have recurrent outbreaks of the same STI, like genital herpes. Recurrent outbreaks can be treated and managed if you know what symptoms to look out for.
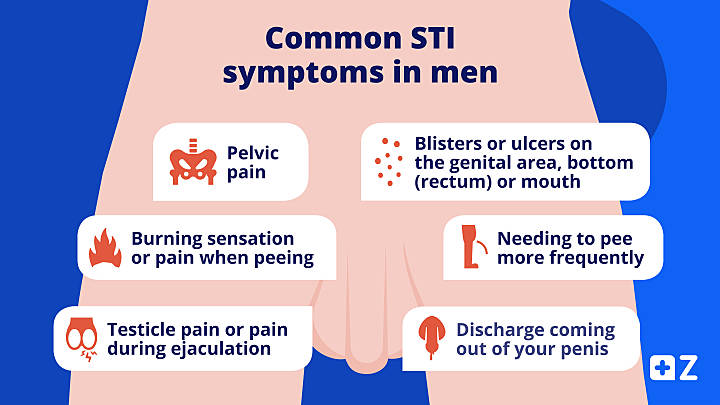
Common STI symptoms in men
You might experience different STI symptoms depending on if you’re a man or a woman. Sometimes you might only have flu-like symptoms, such as feeling fatigued or having aching muscles.
Some common STI symptoms in men include:
- needing to pee more frequently
- burning sensation or pain when peeing
- pelvic pain
- ulcers or blisters on your genital area, bottom (rectum) or mouth
- discharge coming out of your penis
- testicle pain or pain during ejaculation
An STI can cause inflammation in your urethra (the tube where urine and sperm pass through), which is also called urethritis. This can cause problems during sex if you're having difficulty in ejaculating.
If you have an STI, you might have some of these symptoms or no symptoms at all. If you get these symptoms after having unprotected sex, it’s a good idea to get tested for STIs. You can get STI testing kits from ZAVA or at your nearest sexual health clinic.
from £135.99
from £30.99
from £35.99
from £35.99

No results found.
Please check your spelling or try another treatment name.
When do STI symptoms start?
STI symptoms can start anywhere between 1 to 3 weeks after having unprotected sex. Sometimes you’ll get symptoms earlier or later depending on the STI.
Some viruses or bacteria that cause STIs can stay inside your body for a long time and hide from your immune system. A trigger, such as stress or smoking, can cause the virus or bacteria to activate, which is when you’ll start seeing symptoms.
Certain STIs, like HIV (human immunodeficiency virus), can gradually damage your body over time. After you've been infected with HIV you’ll feel like you’ve got the flu for around a week. Even when you get better, the HIV virus will stay in your body. The virus can then damage parts of your immune system without you realising it. A weakened immune system caused by HIV is called acquired immunodeficiency syndrome (AIDS). It can take years between being infected with HIV and getting AIDS.
If you start to feel unwell weeks or months after having unprotected sex, get tested to check for any STIs. It’s also a good idea to get tested if you get a new sexual partner.
What happens if an STI is left untreated?
If you leave an STI untreated you’ll be at risk of getting further health problems. As you won’t always get symptoms when you have an STI, it might be difficult to know if you’ve been exposed. An untreated STI can spread to other sexual partners if you have unprotected sex in the future.
Leaving an STI untreated can also cause infertility, as the quality of your sperm can be affected. For example, gonorrhoea can cause inflammation around your testicles which will affect sperm production. Infertility can happen with several STIs, such as chlamydia and syphilis.
If your partner is a pregnant woman and you pass an STI on to her, this can affect the baby or cause a miscarriage.
Some men can get vaccinated against certain STIs, such as the human papillomavirus (HPV) which causes genital warts. HPV can lead to penile cancer in men and cervical cancer in women. You may want to consider getting a hepatitis B vaccine too to protect your liver.
Nowadays, STIs are easy to treat and treatment is readily available from sexual health clinics. You can also get treatment for different STIs from ZAVA, including chlamydia and trichomoniasis.
Prevention is better than cure, as the saying goes. So it’s a good idea to follow safe sex guidance to protect the health of yourself and others to avoid the complications of STIs.
How to avoid sexually transmitted infections
You can avoid STIs by getting tested regularly, and building a relationship with your partner so that you can trust each other before you start being sexually active. To reduce the chance of getting STIs, practise safe sex by:
- using a barrier method of contraception, such as condoms or a cervical cap
- being honest with your partner about your sexual history
- limiting how many people you have sex with
Remember that STIs can still be passed on to another person through oral sex or anal sex. If your partner has an STI, you should wait until they've been treated and their symptoms disappear completely.
Viral infections such as the herpes simplex virus (which causes genital herpes) can stay dormant in your body. You can still pass genital herpes through skin to skin contact even during the dormant periods, though this is less likely. It's important to communicate with your partner if you know you have herpes and consider tests if you've had unprotected sex.
It’s better to avoid sex when you’re under the influence of alcohol or drugs, as otherwise you’ll be less likely to be aware of having safe sex. Drinking too much alcohol may also lead to problems when having sex, like causing erectile dysfunction.

Dr Babak Ashrafi Clinical Lead for Service Expansion
Accreditations: BSc, MBBS, MRCGP (2008)
Babak studied medicine at King’s College London and graduated in 2003, having also gained a bachelor’s degree in Physiology during his time there. He completed his general practice (GP) training in East London, where he worked for a number of years as a partner at a large inner-city GP practice. He completed the Royal College of GPs membership exam in 2007.
Meet our doctorsLast reviewed: 07 Jan 2022
-
Sexually transmitted infections (NHS) [June 2021] [accessed Nov 2021]
-
How soon do STI symptoms appear? (NHS) [Nov 2019] [accessed Nov 2021]
-
Sexually transmitted diseases (STDs) [Sept 2021] [accessed Nov 2021]
-
HIV and AIDS (NHS) [April 2021] [accessed Nov 2021]
-
7 STIs that affect male fertility [July 2020] [accessed Nov 2021]